Introduction
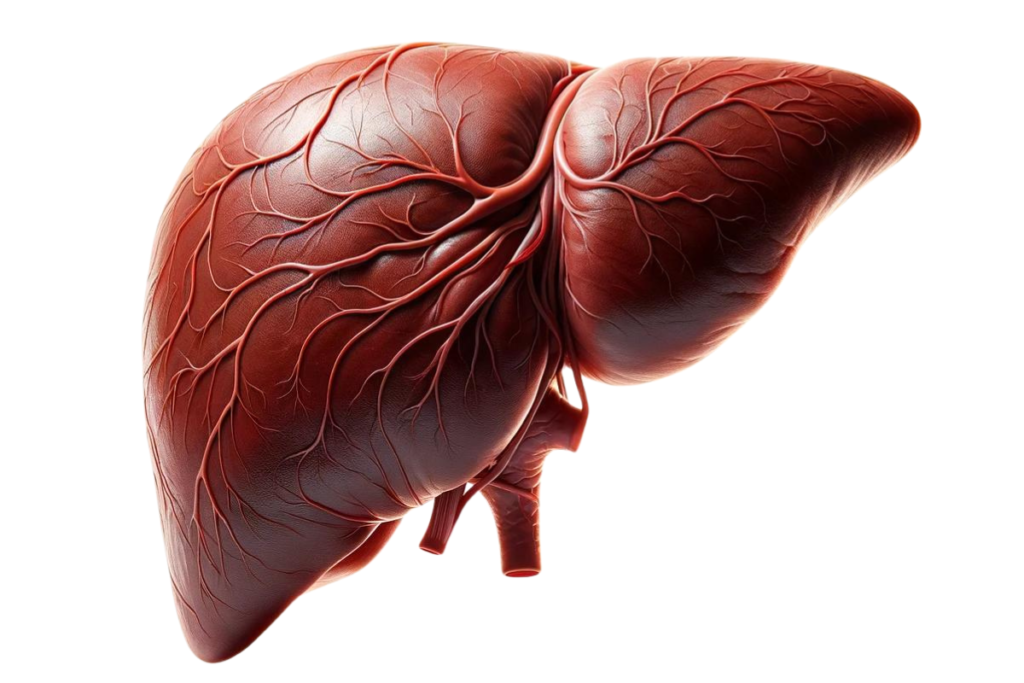
The liver, one of the body’s most vital organs, plays a crucial role in maintaining our overall health. It’s responsible for an array of essential functions, including detoxifying harmful substances, processing nutrients from the food we eat, producing bile to help digest fats, and storing energy in the form of glycogen. Given its central role in our body’s metabolic processes, the health of the liver is paramount to our well-being.
Recognizing liver disease symptoms early on is critical. The liver is remarkably resilient and capable of regenerating itself, but this ability also means that symptoms of disease may not appear until the liver is significantly impaired. Early detection of liver disease symptoms can be the key to preventing irreversible damage, allowing for timely and effective treatment. It’s about understanding the whispers of our body before they turn into screams, ensuring that minor issues don’t escalate into major health crises.
The purpose of this blog post is to shed light on the symptoms associated with liver disease, offering readers a comprehensive guide to understanding these signs. By providing valuable insights into the early and advanced symptoms of liver disease, we aim to empower individuals with the knowledge they need to seek medical advice promptly. Awareness is the first step towards prevention, and through this post, we hope to contribute to a broader understanding of liver health, encouraging proactive measures to maintain it. Join us as we explore the vital signs your liver might be sending you, emphasizing why recognizing these symptoms early can be a lifesaver.
Overview of Liver Diseases
What is Liver Disease?
Liver disease refers to any condition that causes inflammation or damage to the liver, affecting its ability to function properly. It encompasses a wide range of disorders that can impact the liver’s vital processes, including detoxification, metabolism, and the production of essential proteins and bile. The liver’s remarkable ability to regenerate damaged tissue means that early-stage liver disease often goes unnoticed, as there may be no symptoms until the damage is quite advanced.
Types of Liver Disease
There are several types of liver disease, each with its own set of causes and potential impacts on health. The most common include:
- Hepatitis: An inflammation of the liver, usually caused by viral infections (Hepatitis A, B, and C are the most common), but can also result from autoimmune diseases, drugs, toxins, and alcohol.
- Fatty Liver Disease: Characterized by the accumulation of fat in the liver cells, this condition can be non-alcoholic fatty liver disease (NAFLD) or alcoholic liver disease (ALD), depending on the influence of alcohol consumption.
- Cirrhosis: A late-stage liver disease marked by scarring of the liver (fibrosis) and impaired liver function. It’s the result of long-term, continuous damage to the liver and may lead to liver failure.
- Liver Cancer: Primary liver cancer originates in the liver. Hepatocellular carcinoma (HCC) is the most common type. Secondary or metastatic liver cancer has spread to the liver from another organ.
- Autoimmune Liver Diseases: These include conditions like autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis, where the body’s immune system attacks the liver.
Common Causes of Liver Diseases
The causes of liver disease are as varied as the diseases themselves. Some of the most common include:
- Viruses: Viral infections such as hepatitis A, B, and C are leading causes of liver inflammation and disease.
- Alcohol Abuse: Excessive alcohol consumption is a major cause of liver disease worldwide, leading to conditions like alcoholic hepatitis and cirrhosis.
- Genetics: Certain liver diseases, such as hemochromatosis (iron overload) and Wilson’s disease (copper accumulation), are inherited.
- Obesity: Being significantly overweight can lead to non-alcoholic fatty liver disease (NAFLD), a growing concern globally.
- Drugs and Toxins: Some medications, herbal supplements, and toxins can cause liver damage either through direct toxicity or allergic reactions.
- Autoimmune Diseases: Conditions where the immune system attacks the liver can lead to chronic inflammation and liver disease.
Understanding the various types of liver disease and their causes is fundamental to recognizing the risk factors and symptoms associated with each condition. With this knowledge, individuals can take proactive steps towards prevention, early detection, and management of liver disease, preserving their liver health and overall well-being.
Early Symptoms of Liver Disease
The liver plays a pivotal role in numerous bodily functions, including metabolism, digestion, and detoxification. When it begins to falter due to disease, the impact can be subtle and wide-ranging. Recognizing the early symptoms of liver disease can be challenging, as they are often nonspecific and easily mistaken for other health issues. However, understanding these early signs is crucial for timely intervention and treatment.
Fatigue and Weakness
One of the most common yet overlooked symptoms of liver disease is a pervasive sense of fatigue and weakness. This is not the ordinary tiredness that follows a busy day; it’s a profound lethargy that doesn’t improve with rest. The liver plays a crucial role in converting food into energy and removing toxins from the blood. When liver function is compromised, toxin levels can build up, and metabolism can be affected, leading to this profound fatigue.
Loss of Appetite
A diminished appetite is another early sign of liver disease. The liver’s role in digestion and metabolism means that when it’s not functioning correctly, processes that stimulate hunger can be affected. Moreover, liver disease can lead to changes in bile production, essential for fat digestion, which can cause gastrointestinal discomfort and reduce the desire to eat.
Weight Loss
Unexpected weight loss may occur as a direct consequence of a loss of appetite. Additionally, as liver disease progresses, the body may begin to metabolize muscle tissue for energy, further contributing to weight loss. This symptom, especially when unexplained, warrants further investigation to rule out liver disease among other potential causes.
Nausea or Vomiting
Nausea and vomiting can be early signs of liver distress. These symptoms arise because the liver is unable to adequately filter and detoxify the blood, leading to the accumulation of toxins. These toxins can affect the brain’s functioning, known as hepatic encephalopathy, which can cause nausea, vomiting, and even changes in behavior and mood.
Mild Abdominal Discomfort or Pain
The liver is located in the upper right portion of the abdomen, and as liver disease progresses, it can cause swelling and inflammation that result in abdominal discomfort or pain. This pain is typically dull and persistent and may be accompanied by bloating or a feeling of fullness due to fluid accumulation (ascites) or liver enlargement.
Why These Symptoms Appear
These early symptoms manifest because the liver’s impaired function affects the body’s ability to regulate energy, remove toxins, and process nutrients effectively. The buildup of toxins and changes in metabolism can disrupt bodily systems, leading to the general and nonspecific symptoms described. Recognizing these signs as potential indicators of liver disease is critical for early diagnosis and management. Early detection can significantly influence the course of the disease, allowing for interventions that may halt or slow disease progression and minimize liver damage.
Advanced Liver Disease Symptoms
As liver disease progresses to a more advanced stage, the symptoms become more pronounced and severe. These symptoms are indicative of significant liver damage or liver failure and require immediate medical attention. Understanding these signs can help in recognizing the critical need for treatment and potentially life-saving interventions.
Jaundice (Yellowing of the Skin and Eyes)
Jaundice is one of the most recognizable signs of advanced liver disease. It occurs when the liver is unable to process bilirubin, a yellow pigment formed by the breakdown of red blood cells. Normally, the liver filters bilirubin from the blood, converting it into a form that can be eliminated through bile. However, when the liver is damaged, bilirubin accumulates in the body, causing the skin and whites of the eyes to turn yellow.
Swelling in the Legs and Ankles (Edema)
Edema in the legs and ankles is caused by the liver’s inability to produce albumin, a protein that prevents fluid from leaking out of blood vessels into surrounding tissues. Without sufficient albumin, fluid accumulates in the legs and ankles, leading to swelling. This symptom is often exacerbated by an increase in blood pressure in the veins that flow through the liver (portal hypertension).
Swelling in the Abdomen Due to Fluid Accumulation (Ascites)
Ascites is the accumulation of fluid in the abdomen, which can be a sign of severe liver disease. It occurs when the liver fails to synthesize enough albumin and when portal hypertension causes blood to flow less freely through the liver. This combination of factors leads to fluid buildup in the abdominal cavity, causing significant swelling and discomfort.
Itchy Skin
The accumulation of bile salts in the bloodstream can lead to persistent itching (pruritus). This symptom occurs because the damaged liver is unable to efficiently process and eliminate bile, allowing substances that can cause itching to build up in the skin.
Dark Urine Color
Urine may become dark in color due to the increased levels of bilirubin being excreted through the kidneys. This is a direct result of the liver’s reduced capacity to handle bilirubin, forcing the body to find alternative pathways for its elimination.
Pale Stool Color or Bloody, Tar-Colored Stool
A healthy liver releases bile into the intestines, which helps to give stool its normal brown color. Advanced liver disease can lead to pale or clay-colored stools due to a lack of bile. Conversely, bloody or tar-colored stools may indicate bleeding within the gastrointestinal tract, a complication often associated with liver disease and portal hypertension.
Chronic Fatigue
Fatigue in advanced liver disease is more pronounced than the general tiredness experienced in the early stages. It can become debilitating, significantly impacting the individual’s quality of life. This symptom reflects the cumulative effect of the body’s reduced ability to metabolize and detoxify substances, combined with the overall decline in liver function.
Bleeding or Bruising Easily
The liver is responsible for producing proteins necessary for blood clotting. When liver function is severely impaired, there’s a decrease in the production of these clotting factors, leading to an increased tendency to bleed or bruise easily. This can be particularly dangerous as it may lead to significant blood loss from minor injuries.
How These Symptoms Indicate More Severe Liver Damage or Failure
The progression of symptoms from early signs of liver dysfunction to the more severe symptoms outlined above indicates a significant decline in liver health and function. These symptoms reflect the liver’s inability to perform its essential roles, including filtering toxins from the blood, producing vital proteins, and regulating blood clotting and fluid distribution in the body. When these symptoms are present, they often signify advanced liver disease or liver failure, conditions that can have life-threatening consequences without prompt and effective treatment. Recognizing and responding to these signs is crucial for the management and potential stabilization of liver disease.
Complications of Liver Disease
Liver disease, if left untreated or if it progresses significantly, can lead to a range of serious and potentially life-threatening complications. Understanding these complications emphasizes the critical importance of early detection and treatment of liver disease.
Liver Failure
Liver failure occurs when a large part of the liver is damaged beyond repair and the liver can no longer perform its vital functions. It can happen gradually (chronic liver failure) or suddenly (acute liver failure). Symptoms of liver failure include jaundice, easy bleeding, swelling in the abdomen, confusion or disorientation (hepatic encephalopathy), and sleepiness. Liver failure is a medical emergency and requires immediate care.
Liver Cancer
Chronic liver disease and cirrhosis significantly increase the risk of developing liver cancer, particularly hepatocellular carcinoma (HCC), the most common type of primary liver cancer. Liver cancer may not present with noticeable symptoms in its early stages, making it difficult to diagnose early without regular monitoring for those known to have liver disease.
Portal Hypertension
Portal hypertension is a common complication of cirrhosis and is characterized by increased blood pressure in the portal vein system, which carries blood from the intestines and spleen to the liver. This condition can lead to serious complications, including varices (enlarged veins, particularly in the esophagus or stomach, that can bleed heavily) and ascites (accumulation of fluid in the abdomen).
Hepatic Encephalopathy
Hepatic encephalopathy is a decline in brain function that occurs as a result of severe liver disease. In this condition, the liver can no longer adequately remove toxins from the blood, allowing them to build up and affect the brain. Symptoms can range from mild confusion to coma and can be life-threatening.
Kidney Failure
In advanced liver disease, particularly cirrhosis, there is a risk of developing kidney failure, known as hepatorenal syndrome. This severe complication occurs when the kidneys stop functioning properly in response to the changes in blood flow and pressure that accompany severe liver damage.
Increased Risk of Infections
Liver disease can impair the body’s immune response, increasing the susceptibility to infections. This is especially critical in the case of advanced liver disease, where the ability to fight off infections is significantly compromised.
Importance of Early Detection and Treatment
The potential for these severe complications underscores the importance of early detection and treatment of liver disease. Regular medical check-ups and liver function tests can help identify liver disease in its early stages when it’s most treatable. Lifestyle changes, medications, or in some cases, surgical interventions, can effectively manage liver disease if detected early, preventing progression to more severe conditions.
Early treatment can halt or slow the progression of liver disease, reducing the risk of developing these serious complications. For those with advanced liver disease, close monitoring and management can help manage symptoms and improve quality of life. It’s crucial for individuals at risk of liver disease to engage in preventive measures, seek regular medical advice, and adhere to treatment plans prescribed by healthcare professionals.
Section 5: Diagnosing Liver Disease
Diagnosing liver disease early is crucial for effective management and treatment. Various diagnostic tests and procedures are used to evaluate liver function, structure, and to identify the underlying cause of liver disease. Healthcare professionals play a pivotal role in determining the most appropriate diagnostic approach based on the patient’s symptoms, medical history, and risk factors.
Common Diagnostic Tests and Procedures
- Blood Tests: The Liver Function Tests (LFTs) are among the first steps in diagnosing liver disease. These tests measure levels of enzymes and proteins in the blood that indicate liver health, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), bilirubin, and albumin. Abnormal levels can suggest liver damage or dysfunction.
- Imaging Tests: Imaging techniques such as ultrasound, CT (Computed Tomography) scans, and MRI (Magnetic Resonance Imaging) can provide detailed pictures of the liver and help identify abnormalities. An ultrasound is often the first imaging test used, as it can detect liver enlargement, tumors, or signs of certain diseases like fatty liver disease and cirrhosis.
- Liver Biopsy: In some cases, a liver biopsy may be necessary to determine the extent of liver damage and the specific type of liver disease. During this procedure, a small sample of liver tissue is removed with a needle and examined under a microscope. A biopsy can provide definitive information on the degree of inflammation, fibrosis, or cirrhosis.
- FibroScan: Also known as transient elastography, this non-invasive test measures the stiffness of the liver, which can indicate fibrosis or cirrhosis. It’s becoming more common as a less invasive alternative to a liver biopsy for some patients.
- Endoscopy: For patients with symptoms or signs of advanced liver disease, such as varices, an endoscopy may be performed to look for enlarged blood vessels (varices) in the esophagus or stomach that can bleed.
The Role of Healthcare Professionals
Healthcare professionals, including primary care physicians, gastroenterologists, and hepatologists (liver specialists), play an essential role in diagnosing liver disease. They will:
- Assess Symptoms and Medical History: Collect comprehensive information on the patient’s symptoms, alcohol consumption, family history of liver disease, and exposure to potential liver toxins (such as certain medications or chemicals).
- Order and Interpret Tests: Decide which diagnostic tests are necessary and interpret the results within the context of the patient’s overall health and history.
- Provide a Diagnosis: Use the information gathered from symptoms, medical history, and test results to provide a diagnosis.
- Develop a Treatment Plan: Based on the diagnosis, healthcare professionals will formulate a treatment plan tailored to the individual’s specific condition, which may include lifestyle changes, medications, or procedures.
The process of diagnosing liver disease is comprehensive and requires a multidisciplinary approach to ensure accurate diagnosis and effective treatment planning. Early diagnosis and intervention are key to managing liver disease successfully and preventing progression to more severe conditions.
Section 6: Treatment and Management of Liver Disease
The treatment and management of liver disease depend on the type, stage, and cause of the liver disorder. A multifaceted approach involving lifestyle modifications, medication, and, in severe cases, surgical interventions such as liver transplantation, is often necessary. The primary goals are to halt or slow the progression of the disease, manage symptoms, and address any complications that arise.
Lifestyle Changes
- Diet: Nutrition plays a crucial role in managing liver disease. A well-balanced diet rich in fruits, vegetables, lean protein, and whole grains is generally recommended. For certain conditions like fatty liver disease, reducing calorie intake and losing weight can be particularly beneficial. Avoiding foods high in saturated fats, sugar, and salt is also advised.
- Exercise: Regular physical activity helps in maintaining a healthy weight, reducing liver fat, and decreasing the risk of fibrosis in patients with fatty liver disease. It can also improve overall health and well-being.
- Alcohol Intake: For those with liver disease, abstaining from alcohol is crucial, as alcohol can exacerbate liver damage. Even for those with liver disease not directly caused by alcohol, avoiding alcohol can help manage the condition more effectively.
Medication and Treatments for Specific Types of Liver Disease
- Viral Hepatitis: Antiviral medications can be effective in treating hepatitis B and C, potentially curing the infection and preventing further liver damage.
- Autoimmune Hepatitis: Corticosteroids and other immune-suppressing drugs may be used to reduce inflammation.
- Fatty Liver Disease: While there are no specific medications approved for NAFLD or NASH, treating underlying conditions such as obesity, diabetes, and high cholesterol can be beneficial. Research into new treatments is ongoing.
- Cirrhosis: Treatment focuses on managing the symptoms and preventing complications. This may include medications to reduce portal hypertension, prevent bleeding from varices, and manage ascites and encephalopathy.
- Liver Cancer: Treatment options may include surgery, liver transplantation, ablation therapies, embolization therapies, targeted therapy, and immunotherapy, depending on the stage of the cancer and overall liver function.
Potential for Liver Transplantation in Severe Cases
Liver transplantation is considered for patients with end-stage liver disease or liver cancer that cannot be surgically removed. It involves replacing the diseased liver with a healthy liver from a deceased or living donor. Candidates for liver transplantation undergo a comprehensive evaluation process to determine their eligibility. While liver transplantation can offer a chance for a longer, healthier life, it also requires lifelong follow-up and medication to prevent organ rejection.
Management of Liver Disease
Effective management of liver disease involves regular monitoring by healthcare professionals to assess the progression of the disease, adjust treatment plans as necessary, and screen for complications. Education on the condition and its management, support groups, and psychological support can also play vital roles in helping patients cope with their disease.
The management of liver disease is highly personalized, reflecting the diverse nature of liver conditions and the individual circumstances of each patient. Adhering to treatment plans, making lifestyle changes, and maintaining regular follow-up with healthcare providers are key components for successfully managing liver disease.
Section 7: Prevention of Liver Disease
Preventing liver disease is crucial, given the liver’s essential role in numerous bodily functions. While not all liver diseases can be prevented, many can be significantly mitigated through lifestyle choices and preventive measures. Here are key tips for maintaining a healthy liver and the importance of regular medical check-ups.
Tips for Maintaining a Healthy Liver
- Vaccination: Protecting yourself against hepatitis A and B through vaccination is one of the most effective ways to prevent these viral infections that can lead to serious liver diseases. There is currently no vaccine for hepatitis C, but awareness and preventive measures can reduce the risk of infection.
- Avoiding Excessive Alcohol: Excessive alcohol consumption is a leading cause of liver disease. Limiting alcohol intake can prevent conditions such as fatty liver, alcoholic hepatitis, and cirrhosis. Abstaining from alcohol is the best way to reduce the risk of alcohol-related liver diseases.
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support liver health. Avoiding high-calorie meals, saturated fat, refined carbohydrates (such as white bread, white rice, and regular pasta), and sugars can prevent fatty liver disease. Drinking plenty of water is also beneficial.
- Maintain a Healthy Weight: Obesity can lead to non-alcoholic fatty liver disease (NAFLD), which can progress to non-alcoholic steatohepatitis (NASH). Maintaining a healthy weight through diet and regular exercise can significantly reduce the risk.
- Exercise Regularly: Regular physical activity helps to burn triglycerides for fuel and can reduce liver fat.
- Avoid Toxins: Toxins can injure liver cells. Limit direct contact with toxins from cleaning and aerosol products, insecticides, chemicals, and additives in cigarettes.
- Use Medications Wisely: Take prescription and nonprescription drugs only when needed and in recommended doses. Don’t mix medications without the approval of a healthcare provider. Avoid mixing medications with alcohol.
- Practice Safe Sex: Unprotected sex or sex with multiple partners increases the risk of hepatitis B and hepatitis C.
- Be Cautious with Needles: Ensure that any needles used (for tattoos, piercings, or injections) are sterile. Sharing needles can spread hepatitis B, hepatitis C, and HIV.
- Regular Medical Check-Ups: Regular check-ups can help detect liver disease in its early stages, even before symptoms appear. If you’re at higher risk for liver disease, due to factors like a family history of liver disease or heavy alcohol use, regular screening may be advised.
Importance of Regular Medical Check-Ups
Regular medical check-ups are vital for detecting liver disease early and monitoring the health of your liver over time. These check-ups can include blood tests, imaging studies, and physical examinations that assess liver health. Early detection of liver issues allows for timely intervention, which can be crucial in preventing progression to more serious conditions.
In conclusion, the prevention of liver disease involves a combination of vaccinations, lifestyle modifications, and regular medical screenings. By taking proactive steps to protect your liver, you can significantly reduce the risk of developing liver disease and maintain overall health and well-being.
Section 8: Living with Liver Disease
Living with liver disease can present significant challenges, not only in terms of managing the physical symptoms but also in coping with the emotional and psychological effects. However, with appropriate medical care, lifestyle adjustments, and support, individuals with liver disease can lead fulfilling lives. Here’s a guide to managing symptoms, improving quality of life, and accessing support systems and resources.
Managing Symptoms and Improving Quality of Life
- Follow Medical Advice: Adhering to treatment plans and medication schedules prescribed by healthcare professionals is crucial in managing liver disease effectively. Regular follow-up appointments are essential to monitor the condition and adjust treatments as necessary.
- Nutritional Support: Consulting a dietitian to develop a personalized eating plan can help manage symptoms and ensure nutritional needs are met. A balanced diet that supports liver health can significantly impact quality of life.
- Physical Activity: Engaging in regular, moderate exercise can help manage symptoms such as fatigue and depression, improve energy levels, and support overall health. Activities should be tailored to individual capacity and any physical limitations.
- Limit Salt Intake: For individuals experiencing fluid accumulation (ascites), reducing salt intake can help manage swelling and discomfort.
- Manage Fatigue: Pacing activities, taking regular breaks, and ensuring adequate rest can help manage chronic fatigue associated with liver disease.
- Avoid Alcohol and Toxins: Completely avoiding alcohol and minimizing exposure to toxins can reduce liver damage and improve liver health.
- Mental Health Support: Coping with chronic illness can be emotionally challenging. Seeking support from mental health professionals, such as counselors or psychologists, can help manage anxiety, depression, and other emotional aspects of living with liver disease.
Support Systems and Resources for Patients and Their Families
- Support Groups: Joining a liver disease support group can provide emotional support, practical advice, and a sense of community. Sharing experiences with others who understand can be incredibly validating and helpful.
- Educational Resources: Utilizing resources from reputable organizations such as the American Liver Foundation or the British Liver Trust can provide valuable information on liver disease, treatments, and living well with liver conditions.
- Social Services: Social workers can assist in navigating healthcare systems, accessing financial assistance programs, and connecting with community resources.
- Family and Friends: Support from family and friends is invaluable. Open communication about the condition, needs, and ways others can help can strengthen relationships and provide much-needed emotional support.
- Online Forums and Communities: Online platforms can offer support and information sharing for those who may not have access to in-person support groups or prefer the anonymity of online interactions.
Living with liver disease requires adjustments and coping strategies, but it doesn’t mean quality of life must significantly diminish. With the right support and management strategies, many people with liver disease continue to lead active, meaningful lives. Acknowledging the challenges, seeking support, and actively participating in the management of the condition are key steps towards living well with liver disease.
Conclusion
The journey through understanding liver disease, its symptoms, complications, and management highlights the critical importance of recognizing the early signs that something may be amiss with one of the body’s most vital organs. The liver’s ability to silently endure considerable damage before symptoms become apparent underscores the necessity of vigilance and awareness in preserving liver health.
Recognizing symptoms—ranging from the subtle indications of early liver disease to the more pronounced signs of advanced conditions—is more than an exercise in health literacy; it’s a crucial step in safeguarding one’s well-being. Early detection can make a significant difference in the outcome, enabling interventions that can halt or slow disease progression, manage symptoms effectively, and prevent serious complications.
We strongly encourage anyone experiencing symptoms suggestive of liver disease not to dismiss them as inconsequential. Seeking medical advice promptly can open pathways to diagnostic clarity and appropriate treatment, offering the best chance for a positive health outcome. It’s essential to engage with healthcare professionals who can provide guidance, support, and the necessary care tailored to individual health needs.
Awareness and early intervention are powerful tools in the fight against liver disease. By fostering a deeper understanding of liver health, encouraging proactive health management, and emphasizing the importance of regular check-ups, we can collectively contribute to the early detection and effective management of liver disease. Let this knowledge empower you to take control of your liver health, advocate for your well-being, and support others in recognizing the importance of liver disease awareness.
In closing, the journey to maintaining liver health is a proactive one, filled with informed choices, timely actions, and the unwavering support of healthcare professionals, family, and community resources. Together, let’s prioritize liver health and embrace the practices that support it, ensuring a healthier future for ourselves and those around us.
As we conclude our comprehensive journey through the realm of liver health, we recognize the power of knowledge and the significant impact it can have on our lives and the lives of those around us. Liver disease, with its myriad forms and complexities, is a prevalent issue that demands attention, understanding, and action. But awareness is the first step towards change, and each of us holds the key to unlocking a healthier future.
Spread Awareness: We encourage you to share this post with your friends, family, and wider network. By spreading the word about liver disease, its symptoms, and the importance of early detection, you contribute to a greater awareness that can potentially save lives. Social media, email, or simply discussing the topic in your community can make a profound difference. Remember, knowledge shared is power multiplied.
Seek Professional Advice: If you or someone you know is experiencing symptoms related to liver disease, or if there are concerns about liver health, we strongly urge you to consult a healthcare provider. Healthcare professionals can offer personalized advice, conduct necessary screenings, and provide guidance tailored to individual health needs. Taking action by seeking professional advice is a critical step in ensuring your health and well-being.
Your health is your most valuable asset, and taking proactive steps to protect it is of utmost importance. Let’s take this knowledge and use it to foster a culture of health awareness and proactive living. By sharing this information and encouraging dialogue on liver health, we can help build a foundation for healthier communities.
Together, we can make a difference. Share this post, talk about liver health, and remember, when it comes to your health and the health of your loved ones, it’s always better to act sooner rather than later. Let’s join hands in spreading awareness and encouraging proactive health management. Your voice matters—let it be heard.
